About Leg Veins
The circulatory system is made up of both veins and arteries. Arteries delivers fresh oxygen rich blood from the heart to all tissues and veins then collect the oxygen-depleted blood again and transport it back to the heart.
The heart will pump blood through the arteries, but not all the way through the veins.
In the lower limbs, blood requires a different transport system to return it, against gravity, back to the heart. This transport system is made up of a pump again, the “calf pump” and one way valves within the veins.
It is for this reason that walking is a great way to keep your legs healthy, since the calf pump is activated all the time.
Broken one-way valves in the legs will cause blood to flow back through the vein and pool in the lower legs, this is known as venous reflux, and often presents as varicose veins. Varicose veins are large blue tortuous vessels that buldge from the surface of the skin.
Varicose Veins
What are varicose veins?
One-way valve failure in the major superficial leg veins (the saphenous veins) is the most common cause of vein reflux and causes varicose veins in other parts of the leg. Typically, veins visible in the lower thigh, knee and calf are often due to vein reflux in higher areas of this major superficial vein. Venous reflux stretches the vein and puts additional pressure on the other healthy valves. The result is varicose veins that appear as tortuous, enlarged blue veins that bulge from the surface of the skin. It is important to understand that the varicose veins that you see on the surface of the skin are in fact branches of the incompetent major superficial leg veins. Varicose veins in the legs are common and affect 3 in 10 people in the general population, typically between the ages of 30 and 70. They prevent blood clearing effectively from your legs, and causes symptoms of veins. Women seek treatment more often than men for their varicose veins.
Varicose veins symptoms
Varicose veins symptoms are varied. Some patients might be asymptomatic or not have any symptoms due to their veins. Common symptoms of varicose veins include leg pain, swollen ankles and feet, itching, heavy legs, tired and aching legs especially towards the end of the day or after prolonged periods of standing or sitting.
More severe symptoms include skin changes like darkening around your ankles(pigmentation), chronic inflammation, dry, scaling skin, leg swelling and calf pain. Symptoms that warrant an immediate visit to a vein specialist or vein doctor include open sores or bleeding from varicose veins.
Varicose veins causes
The exact cause of varicose veins is not yet known. There are however a number of risk factors that contribute to the weakening of vein walls, which in turn leads to the failure of one way valves within the veins:
Studies have shown that increasing age, female sex, childbirths, standing posture at work, higher weight or height, and positive family history are significantly associated with varicose veins1 . Familial predisposition is an important association with varicose veins, but less important than previously thought2. Women are more likely to suffer from abnormal leg veins. Hormonal factors including puberty, pregnancy, menopause, the use of birth control pills, estrogen, and progesterone affect the disease. It is very common for pregnant women to develop varicose veins during the first trimester.
Pregnancy causes an increases in hormone levels and blood volume which in turn, cause veins to soften and enlarge, leading to temporary or permanent valve failure. In addition, the pregnant uterus within the pelvis causes andobstruction to bloodflow and an increased pressure in the veins.
Varicose veins due to pregnancy often improve within 3 months after delivery, even in severe cases. However, with successive pregnancies, abnormal veins are more likely to remain.
Other predisposing risk factors include aging, obesity, leg injury and standing occupations like teachers, pharmacists, and nurses.
In rare cases, anomalies and disease of the important large veins in the abdomen may cause varicose veins3. In these cases treatment of the varicose veins is not possible and would be harmful to the patient. It is important to always consult a specialist regarding your treatment.
Varicose veins complications
Varicose vein complications are many and varied. The severity of problems assosciated with them does not always match the visually obvious problem. Patients with small varicose veins may complain of significant associated pain, while others with large varicose veins will often have no symptoms. All patients however will report improvement in the way their legs feel after treatment. Patients with venous reflux in both legs, often do not know what normal legs should feel like and just assume everyone's legs feel the same.
Ulcers
The most severe varicose vein complication is a venous leg ulcer. As oxygen-poor blood pools in the lower legs, tissues are deprived of neccessary oxygen and nutrients. Small skin injuries takes much longer to heal and eventually will fail to heal and become an ulcer.
These ulcers are usually progressive and will enlarge over time. Patients can have ulcers that fail to heal over several years. This is a very morbid condition, as the ulcer takes presedence over anything else in that patient's life. In a very small group of patients, these ulcers can even result in cancerous skin changes.
Successful ulcer treatment is highly dependant on treating the underlying cause, namely the venous reflux or leaky valves. Failing to treat the underlying cause will lead to poor results. By only using dressings and compression stockings, some ulcers will heal and then recur at a later stage, and often enter a cycle of healing and recurring over weeks to months. Various studies have now proven that ulcer patients should NOT be offered compression treatment as the first choice. Current international guidelines confirm that all ulcer patients should be referred for a duplex doppler scan. Should venous reflux be found, then this has to be treated, and the preferred treatment is endovenous thermal ablation - ie. Radio Frequency ablation.
Feb, 2014 Venous leg ulcer
71 year old male patient with a chronic venous ulcer of the ankle area. Present for 8 years prior to treatment.
Read More about Venous UlcersVenous Eczema
Venous eczema is very similar to normal eczema and can occur in patients with or without a history of eczema elsewhere. The pooling of blood again plays a central role.
I often tell patients that venous eczema is an SOS from your skin. Topical steroid creams will often clear an acute episode, but will recur at a later stage. Skin moisturisers will lessen the chance of an outbreak. The only longterm cure is treating the underlying venous reflux.
Jan, 2014 Venous eczema
41 year old male patient with chronic venous eczema of the ankle area. Present for more than 10 years years prior to treatment.
Skin Itch
In large population studies this seemingly insignificant symptom has been shown to be the most reliable predictor of more severe varicose vein complications. The symptom represents the skin becoming more dry as it becomes less well nourished.
Leg Pain
Many people with varicose veins, whether large or small will complain of pain as one or the only one of their varicose vein symptoms. Venous reflux associated leg pain follows a characteristic pattern. Legs feel fine in the morning and become more and more painful and heavy as the day goes on. Pain is often exacerabted by prolonged standing, hot weather or female menses.
It may be present as a dull ache. Some patients will only experience pain on going to bed at night. Elevating the legs will improve this symptom. If leg elevation worsens your leg pain, then you might have a problem with the arteries in your leg. With more advanced vein disease patients will experience pain as soon as they put their legs on the floor. The blood flowing the wrong way down their enlarged veins, rushes to their lower legs and feet as they stand up.
Superficial Blood Clots / Superficial Thrombophlebitis
This common complication of varicose veins will occur either spontaneously or after minor trauma. Varicose veins may become hard, tender to touch, or even red, warm and tender without touch. This is usually a localized superficial clot within the vein. This is NOT the same as a deep vein thrombosis and does not carry the same risk.
Sluggish and turbulent blood flow in varicose veins, predisposes the blood to clot. The redness and tenderness indicates an inflammatory reaction or your body breaking down the clot. This is not an infection, and usually do not require an anti-biotic.
These localised clots very rarely will extend into deeper veins and cause further complications.
Read More about Superficial Thrombophlebitis
Cramping
Night time cramps, particularly if they occur regularly, are one of those varicose vein complications that people often do not associate with their veins. Cramping in the feet is often reported by vein patients.It is likely caused by local muscle irritability from increased waste products present in the sluggishly moving blood.
Restless Legs
Restless legs with the inability to keep from moving legs with prolonged sitting or standing can occur as one of the many varicose vein complications. It tends to occur more towards the end of the day and can affect patients going to bed. It is likely caused by fluid retention within the tissues.Leg / Ankle Swelling
More severe varicose veins are associated with swelling of the ankles usually towards the end of the day. It is important to note that there are a number of other causes of leg swelling.Lipodermatosclerosis
This is one of the more severe and non-reversible varicose vein complications. The skin around and just above the ankles becomes hardened, tough and discoloured. It represents chronic scar or fibrous tissue replacing healthy sub-cutanous fat in the skin due to long term poor nutrition and back pressure injury from venous reflux. Some patients develop an inverted champagne glass appearance to their legs where the tissue contracts down and skin above bulges. Acute LDS presents as acutely inflammed skin - red, warm and tender. Often misdiagnosed and treated with anti-biotics. Acute LDS indicates skin at risk and requires further investigation and treatment.Jun, 2013 Lipodermatosclerosis
Venous reflux leading to lipodermatosclerosis
Bleeding Varicose Veins
One of the more dramatic, but easily treated, vein complications is bleeding occurring with relatively little or no apparent injury to the skin. It often happens in the bathroom following a bath or shower. The skin is thin and weak and bleeding from a pressurized vein ensues. Immediate treatment is as simple as elevating the leg and applying local pressure at the bleeding point. This can then be converted to a pressure dressing. Further investigation and treatment by a vein specialist is required.Tired and heavy legs
Tired and heavy legs are often reported after prolonged standing. Some patients will even avoid standing in queues due to the ensuing pain. Treatment of the enderlying venous reflux will cause this symptom to resolve. Temporary relief can be obtained by wearing class 2 graded compression stockings.Varicose veins treatment
Varicose veins are treated with lifestyle changes and medical procedures. The goals of treatment are to relieve symptoms, prevent complications, and improve appearance. With the advent of advanced modern day treatments, lifestyle changes are now used as an adjunct in treatment and not a mainstay treatment as in the past. Implementing lifestyle changes only, will not remove varicose veins. If your varicose veins are symptomatic, you will likely require a medical procedure. Some people who have varicose veins choose to have procedures to improve how their veins look.
Lifestyle Changes
Simple lifestyle changes can assist in reducing pain and other symptoms of varicose veins.
Medical Procedures
Modern medical procedures for veins are done to close them. Removing or closing varicose veins usually does not cause problems with blood flow, because the blood starts flowing through other healthy veins. You may be treated with one or more of the procedures described below. Common side effects right after most of these procedures include mild bruising, swelling, skin discoloration, and slight pain.
Venefit™ - Radio Frequency Ablation
Endovenous radio frequency ablation is a technique whereby faulty veins are thermally ablated from the inside out. It involves inserting a thin wire / catheter into the faulty vein and under local anesthesia delivering a controlled amount of heat energy to destroy the inner lining of the vein. This is a very safe and highly effective treatment for varicose veins and represents the treatment of choice in our vein centres.
Read More about Venefit™EVLA - Endovenous Laser Ablation
Endovenous laser ablation is a technique whereby faulty veins are thermally ablated from the inside out. It involves inserting a thin wire / catheter into the faulty vein and under local anesthesia delivering a controlled amount of heat energy to destroy the inner lining of the vein. This is a very safe and highly effective treatment for varicose veins. The technique is very similar to the Venefit procedure, except that laser energy is used.
Read More about EVLAUltrasound Guided Foam Sclerotherapy
Ultrasound guided foam sclerotherapy is a highly effective sclerotherapy technique to treat small varicose veins. Ultrasound is used to direct the injection of foam sclerotherapy directly into the required vein. Hence the name “ultrasound guided foam sclerotherapy"
Read More about USGFSCosmetic sclerotherapy
Cosmetic sclerotherapy is the technique used to treat spider veins of the legs. It is a simply procedure which involves injecting a liquid into the spider veins which destroys them and causes them to disappear over time. It is suitable for use on spiderveins on the legs. Facial veins are better treated by a dermatologist using Electro Surgery, Intense Pulsed Light (IPL) or laser.
Read More about Cosmetic SclerotherapyVenaseal™ - Glue treatment
The Venaseal™ or superglue treatment is a new way of closing the main vein in the leg that causes varicose veins. When this procedure is performed, only one needle hole is needed per vein treated as there is no need for the additional injections of local anaesthetic around the vein – unlike endovenous laser ablation or radiofrequency ablation. Venaseal is a very new treatment.
Read More about Venaseal™Clarivein™ - mechanical chemical ablation
Clarivein is a new system where a catheter with a rotating tip is inserted into the vein and while the tip is rotating in the vein, a chemical solution is injected into the vein. This treatment also requires no local anesthetic injections around the vein.
Read More about Clarivein™Varicose veins prevention
Our current understanding of varicose veins would suggest that you cannot prevent varicose veins from forming. However, you can prevent the ones you have from getting worse. You also can take steps to delay other varicose veins from forming. These measures are the same as listed above in lifestyle changes.
Varicose Veins Diagnosis
Venous duplex ultrasound scanning is the current gold standard in the diagnosis of vein disease. It involves the use of an ultrasound machine and high frequency probe to accurately asses the anatomy of your veins as well as the flow patterns wihin them. Ultrasound scanners do not produce any radiation (unlike x-rays) and they don’t involve needles or injections. We do not use the older techniques like the Trendelenburg or tourniquet test to diagnose vein disease. Hand-held dopplers are not used in our vein centres as they are inaccurate.
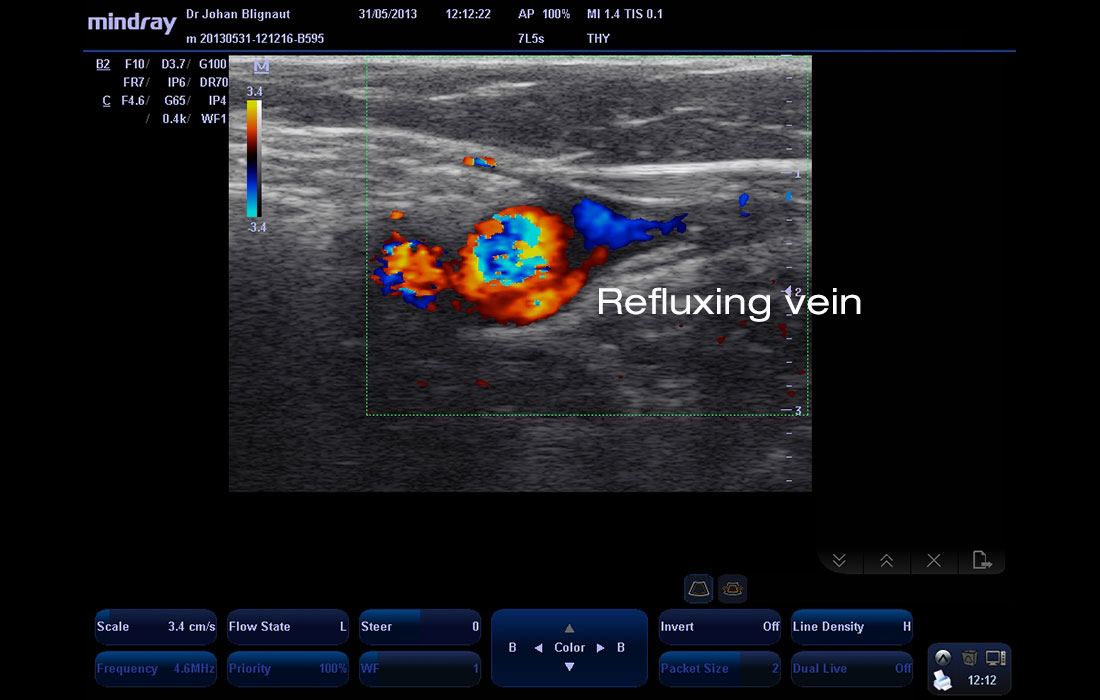
Jun, 2013 Colour Duplex Image
Colour Duplex doppler image of refluxing greater saphenous vein
1. Risk indicators for varicose veins in forty- to sixty-year-olds in the Tampere varicose vein study.
World J Surg. 2002 Jun;26(6):648-51. Epub 2002 Mar 1 >
2. Effect of family history on the incidence of varicose veins: a population-based follow-up study in Finland.
Angiology. 2009 Aug-Sep;60(4):487-91 >
3. Varicose veins: look before you strip - the occluded inferior vena cava and other lurking pathologies.
S Afr Med J. 2014 May 15;104(10):668-70. doi: 10.7196/samj.8395>